Can Malaria be Transmitted Through Blood Transfusion

Did you know that blood transfusions are among the eight most crucial lifesaving interventions in emergency and maternal care? They are used for many different reasons, and the total amount of blood transferred exceeds 14 million units annually in the U.S. These include treatment for anemia, post-surgery, childbirth complications, and cancer. Certain dangerous diseases like HIV, hepatitis, or syphilis can be transmitted through blood and are therefore screened for before each blood transfusion. But have you ever wondered whether malaria can be transmitted through blood transfusion? This article will help you find the answer to this question, understand what malaria is, and how to prevent and treat this disease.
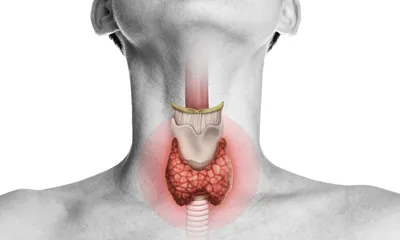
What is Malaria?
Malaria is a parasitic infection with around 263 million cases globally in 2023. It's most common in hot, humid, rainy, and low altitude regions such as parts of Africa, as well as other tropical and subtropical regions in Asia, the Middle East, and South America. As one of the most fatal diseases worldwide, it causes around 600.000 deaths every year, especially among young children aged five or younger.
The disease is mosquito-borne and caused by Plasmodium, a group of parasites, which is transmitted to humans by the bite of infected female Anopheles mosquitoes. There are multiple species, including the most dangerous, P. falciparum. Other types like P. vivax and P. ovale can remain dormant in the liver, causing relapses months or even years after the initial infection. The symptoms of malaria include fever and chills, headache, muscle pain, vomiting, and tiredness.
Can Malaria be Transmitted Through Blood Transfusion?
While malaria can be transmitted through blood transfusions, this rarely occurs in countries with highly regulated blood bank systems, such as the U.S. or Canada. However, it’s a serious concern in high-risk areas that often have limited resources. This is especially true because screening for the infection is usually less straightforward than for other serious diseases like HIV, since the infection level can be too low for detection.
When infection through a blood transfusion, also called transfusion-transmitted malaria (TTM), does occur, it’s often more severe than when caused by a mosquito bite, and symptoms tend to appear more quickly. This occurs because the infection enters the bloodstream directly, bypassing the liver, particularly since blood transfusions are usually given to individuals who are already weakened or ill. Blood donation centres often try to prevent this type of transmission by temporarily deferring individuals who have recently travelled to or resided in malaria-endemic regions.
How to Prevent and Treat Malaria
Malaria prevention has two main pillars: preventing mosquito bites and vaccination. For example, bed nets, protective clothing, mosquito repellent, and indoor residual spray are commonly used in high-risk regions. Two malaria vaccines are also available, designed to protect children in endemic regions. Additionally, preventive antimalaria drugs, such as Malarone or Acticlate are recommended for travellers or vulnerable people.
After a malaria infection has been detected, the treatment depends on the severity of the disease and the Plasmodium species detected. While artemisinin-based combination therapies are often used for mild P. falciparum malaria cases, severe infections usually require immediate treatment and often hospitalization. In these instances, artesunate is frequently given intravenously. Finally, to successfully treat non-falciparum malaria, drugs like Chloroquine or Primaquine are used.
IMPORTANT NOTE: The above information is intended to increase awareness of health information and does not suggest treatment or diagnosis. This information is not a substitute for individual medical attention and should not be construed to indicate that use of the drug is safe, appropriate, or effective for you. See your health care professional for medical advice and treatment.